Overview
- Hydrops fetalis or fetal hydrops is a lethal fetal condition defined as abnormal accumulation of fluid in two or more fetal compartments presenting as ascites, pleural effusion, pericardial effusion and skin edema. It may also be associated with polyhydramnios and placental edema. Hydrops is usually detected using ultrasound in the first or second trimester of pregnancy. The etiology can be immune or nonimmune. Immune hydrops fetalis is due to Rhesus (Rh) or ABO incompatibility and other blood group antibodies causing hemolytic disease of the newborn. Nonimmune hydrops fetalis can be divided as fetal, maternal, placental and idiopathic. A wide spectrum of genetic causes may lead to nonimmune hydrops fetalis (NIHF), and so a phenotypic and genetic evaluation are necessary to determine the underlying etiology. The mode of inheritance is generally autosomal recessive and autosomal dominant, although several X-linked related pathologies have been identified.
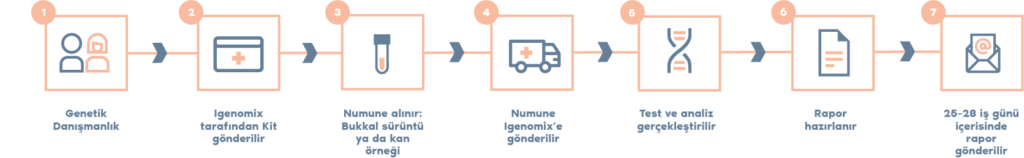
- The Igenomix Hydrops Fetalis Syndrome Precision Panel can be used to make a directed and accurate diagnosis ultimately leading to a better management and prognosis of the disease. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved.
Indication
- The Igenomix Hydrops Fetalis Syndrome Precision Panel is indicated for those patients with ultrasound findings suggestive of hydrops fetalis or with the following manifestations:
- Twin pregnancy
- Previous fetal death
- Prolonged or excessive jaundice in siblings as newborns
- Family history of genetic disorders, chromosomal abnormalities, or metabolic diseases
- Polyhydramnios or oligohydramnios
- Evidence of viral illness in mother or fetus
- Decreased fetal movements
- Fetal tachyarrythmias
- Maternal history of: Rh negative blood type, known presence of isoimmune blood group antibodies, illicit drug use, collagen vascular disease, blunt abdominal trauma, coagulopathy, hemoglobinopathy etc
Clinical Utility
The clinical utility of this panel is:
- The genetic and molecular confirmation for an accurate clinical diagnosis of a symptomatic patient.
- Early initiation of treatment in the form early referral to a high-risk center, multidisciplinary counselling and close coordination between obstetric and neonatal specialists or early invasive fetal treatment.
- Risk assessment of asymptomatic family members according to the mode of inheritance.
- Improvement of delineation of genotype-phenotype correlation.
References
Waring, G. J., Splitt, M., & Robson, S. C. (2019). Fetal hydrops: diagnosis and prognosis. Archives of disease in childhood, 104(3), 209–210. https://doi.org/10.1136/archdischild-2018-315777
Mardy, A. H., Chetty, S. P., Norton, M. E., & Sparks, T. N. (2019). A system-based approach to the genetic etiologies of non-immune hydrops fetalis. Prenatal diagnosis, 39(9), 732–750. https://doi.org/10.1002/pd.5479
Bellini, C., & Hennekam, R. (2012). Non-immune hydrops fetalis: A short review of etiology and pathophysiology. American Journal Of Medical Genetics Part A, 158A(3), 597-605. doi: 10.1002/ajmg.a.34438
Sparks, T. N., Thao, K., Lianoglou, B. R., Boe, N. M., Bruce, K. G., Datkhaeva, I., Field, N. T., Fratto, V. M., Jolley, J., Laurent, L. C., Mardy, A. H., Murphy, A. M., Ngan, E., Rangwala, N., Rottkamp, C., Wilson, L., Wu, E., Uy, C. C., Valdez Lopez, P., Norton, M. E., … University of California Fetal–Maternal Consortium (UCfC) (2019). Nonimmune hydrops fetalis: identifying the underlying genetic etiology. Genetics in medicine : official journal of the American College of Medical Genetics, 21(6), 1339–1344. https://doi.org/10.1038/s41436-018-0352-6
Désilets, V., Audibert, F., Wilson, R., Audibert, F., Brock, J., & Carroll, J. et al. (2013). Investigation and Management of Non-immune Fetal Hydrops. Journal Of Obstetrics And Gynaecology Canada, 35(10), 923-936. doi: 10.1016/s1701-2163(15)30816-1
Jauniaux E. (1997). Diagnosis and management of early non-immune hydrops fetalis. Prenatal diagnosis, 17(13), 1261–1268. https://doi.org/10.1002/(sici)1097-0223(199712)17:13<1261::aid-pd292>3.0.co;2-c